- Blood plays a vital role in the health of the body, however, some people have blood disorders that cause blood not to act as it should.
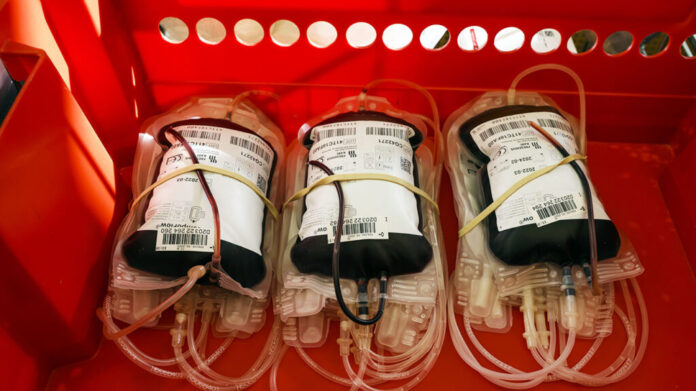
- A team of researchers led by the National Health Service (NHS) Blood and Transplant unit recently launched the first clinical trial to transfuse lab-grown red blood cells into a live human.
- Researchers hope the manufactured red blood cells will help people with rare blood types and disorders such as sickle cell disease.
Blood is an extremely important fluid in the body. Not only does it carry vital nutrients and oxygen to all the body’s organs, but it also helps remove waste and fights infections.
Sometimes a person may have a blood disorder causing their blood to not act as it should. One of these disorders is sickle cell disease, which affects the body’s
There are different types of blood and some are rarer than others. People can have rare blood types that make transfusion difficult if they are in an accident or need surgery. For example, AB negative is the rarest blood type with only 1% of the general population having it.
To help combat these issues, a team of researchers led by the United Kingdom’s National Health Service (NHS) Blood and Transplant (NHSBT) unit recently launched the first clinical trial to ever transfuse laboratory-grown red blood cells into a live human.
If proven to be safe and effective, researchers hope these manufactured red blood cells can aid those with rare blood types and blood disorders like sickle cell disease.
Blood is made of a liquid called plasma and has three main types of cells:
Red blood cells are made in the bone marrow which is found in the middle of most bones. The bone marrow contains stem cells that can become red blood cells, white blood cells, or platelets.
The main job of red blood cells is to carry oxygen throughout the body. Red blood cells contain a protein called hemoglobin, which carries oxygen. Iron from our diet is a major component of hemoglobin.
If a person has a low red blood cell count, they can become anemic, they may experience fatigue, lightheadedness, and other issues. The most common form of anemia is iron deficiency anemia, which can be resolved through dietary changes and supplements.
Sickle cell disease can also cause anemia. If a person has sickle cell anemia, their red blood cells — which are normally shaped like a doughnut without the hole punched out — become C-shaped. This stops the hemoglobin from carrying oxygen as efficiently.
The cells also become very sticky and inflexible, causing them to clump and block blood vessels. Additionally, sickle cells do not live as long as healthy red blood cells, causing a shortage of red blood cells in the body.
A team of researchers has been working on growing red blood cells in a laboratory setting since 2009.
Dr. Cedric Ghevaert, professor in transfusion medicine and consultant hematologist at the University of Cambridge and NHS Blood and Transplant, and co-chief investigator of this clinical trial said they decided to grow red blood cells in a lab because they “knew this technology may help patients with [a] rare blood group for whom it is difficult to find compatible blood donors, and for patients with lifelong transfusion needs for whom red cells with a longer half-life would be hugely beneficial.”
For example, Dr. Ghevaert said they can grow red blood cells from stem cells that carry very rare blood groups.
According to a spokesperson for NHSBT, to grow red blood cells in a laboratory setting, they use stem cells from donors, which they isolate from a standard donation of whole blood. The stem cells are then placed in a nutrient solution.
Over 18–21 days, the solution encourages the cells to multiply and develop into more mature cells. Researchers require 24 liters of nutrient solution and cells to filter out one to two tablespoons of red blood cells.
This process results in
The final product is then stored and refrigerated for up to 10 days in a small sterile vial used for storing red blood cells for transfusion.
In this clinical trial, researchers will take the laboratory-made red blood cells and transfuse them into a live human.
Two people have reportedly already received transfusions of lab-grown red blood cells without any complications. For this study, a minimum of 10 people will receive two mini transfusions — one of the standard donated red blood cells and another of lab-grown cells — at least 4 months apart.
Dr. Ghevaert said one of the main purposes of the trial is to see if the lab-grown red blood cells survive in the body as long as standard donated blood cells:
“If they last longer in circulation then we could transfuse our patients far less often — currently every 2 to 3 weeks intervals, looking to extend to 6 weeks — which means they don’t accumulate iron as much. Iron in the long term is toxic and it’s difficult to excrete the iron that comes with the transfused red cells, so transfusing less often is important.”
According to a spokesperson for NHSBT, further trials are needed before clinical use, but this research marks a significant step in using manufactured blood to improve treatment for patients with rare blood types.
“It will be years before lab-grown blood can be used outside of trials and the vast majority of patients will continue to rely on the generosity of blood donors for the foreseeable future,” the spokesperson told us.
“Introducing new treatments can take anything between 5 to 15 years. This is the first of many stages of testing on humans needed,” they explained.
Medical News Today also spoke with Dr. Lewis Hsu, chief medical officer of the Sickle Cell Disease Association of America, and professor of pediatric hematology at the University of Illinois at Chicago about this clinical trial.
He commented that this new study is exciting because it is another milestone in the long journey of developing lab-grown red blood cells.
“Blood for transfusion relies upon donations from people,” Dr. Hsu said when asked about the importance of being able to use lab-grown red blood cells for transfusions.
“Blood donors need to be healthy and willing to donate. Donated blood has a limited shelf life and then it is no longer useful. [And] the blood cells need to be matched so that the recipient’s immune system does not reject it,” he explained.
“Some people have rare blood types and have few donors who match,” he continued. “This immune reaction to transfused blood is a frequent problem for individuals with sickle cell disease, worldwide. We have to push for extra blood drives to recruit donors for sickle cell patients and sometimes that is not enough blood units.”
As for the next research steps, Dr. Hsu said as the test doses in the clinical trial are about a teaspoon, they are not yet useful for transfusion. Additionally, the laboratory-grown red blood cells would need to tick a number of boxes, including the ability to be produced on a large scale, practical storage, and reasonable cost.
“We also note that huge scientific progress has been made in reducing the need for blood transfusions, which is a strategy called
“Better surgical techniques reduce blood loss in the operating room, including salvaging and ‘recycling’ some blood back into the patient. Patients with trauma — car crashes, gunshot wounds, industrial accidents — have better monitoring of clotting function that fine-tune the way to stop bleeding and reduce transfusions. New medicines can correct anemia or reduce bleeding. And we have learned what level of anemia under what conditions can be tolerated by the body without a blood transfusion.”
– Dr. Lewis Hsu
Hits: 0