- Scientists from Cambridge University conducted a trial using an artificial pancreas in people with type 2 diabetes.
- The artificial pancreas is a closed-loop system that consists of an insulin pump and glucose monitor, and they link to an app the researchers developed.
- By the end of the trial, the participants who used the artificial pancreas stayed in their target glucose range for twice as long as they did without the artificial pancreas.
Researchers from the Wellcome-MRC Institute of Metabolic Science at the University of Cambridge in the United Kingdom developed an artificial pancreas that they tested on patients with type 2 diabetes who were in end-stage renal failure and on dialysis.
After the artificial pancreas worked well with this group, the researchers wanted to learn whether it could be effective in other people with type 2 diabetes.
With the number of people living with type 2 diabetes increasing, researchers are looking for more efficient treatments, and they hoped this approach provide another option.
The results of the study appear in
Type 2 diabetes is a metabolic disorder that occurs when the body cannot process insulin properly. Insulin is a hormone produced by the pancreas.
According to the
Unhealthy eating habits and lack of physical exercise often lead to a person developing obesity, which can contribute to developing type 2 diabetes.
Sometimes making healthier lifestyle changes can improve the symptoms, but other times people with type 2 diabetes may need to take medications to keep their blood sugar levels stable.
The CDC notes that around 37 million people in the United States have diabetes, with 90–95% of these cases being of type 2 diabetes.
This study follows a
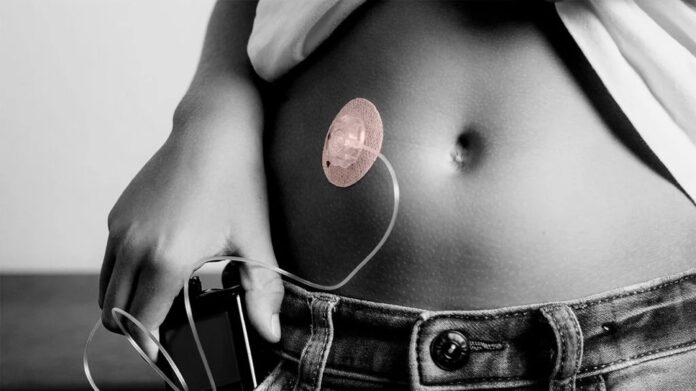
The artificial pancreas is not an artificial organ that requires surgical implantation, but a technological device the user wears on the body that mimics how the pancreas works.
The artificial pancreas combines an insulin pump and glucose monitor, which link to an app that uses an algorithm to analyze blood glucose levels and deliver insulin as needed to keep levels stable.
Since the researchers saw good results with the patients on dialysis, they wanted to see how the artificial pancreas would work with people with only type 2 diabetes.
The researchers studied a group of 26 people with type 2 diabetes. The scientists divided the participants into two groups.
The first group used the artificial pancreas for 8 weeks and then switched to 8 weeks of standard therapy. The second group started by receiving standard injection therapy for 8 weeks and then switched to the artificial pancreas.
The goal was to see how much time patients of each group spent with their glucose in the target range of 3.9 and 10 millimoles per liter (mmol/L), the glucose range
The artificial pancreas delivered the best results for staying within the target glucose range. Patients with the artificial pancreas stayed within the target range 66% of the time, compared to just 32% when using standard injection therapy.
While patients used the artificial pancreas, they spent an additional 8 hours per day in their target glucose range.
“The present study shows that fully closed-loop insulin delivery is a safe and effective approach to improve glycemic control in people with type 2 diabetes during 8 weeks of use in the outpatient setting,” write the authors.
The authors noted that one area of concern using an artificial pancreas was the risk of hypoglycemia, which is when the body’s blood sugar is too low. However, this did not happen.
“We have shown that fully closed-loop insulin delivery does not increase the risk of hypoglycemia,” note the authors.
Co-lead author of the study Dr. Charlotte Boughton points out that “[m]any people with type 2 diabetes struggle to manage their blood sugar levels using the currently available treatments, such as insulin injections.”
“The artificial pancreas can provide a safe and effective approach to help them, and the technology is simple to use and can be implemented safely at home,” she adds.
Dr. Boughton also spoke about the study in an interview with Medical News Today. She explained what comes next for the device:
“Our main message from this study is that this fully automated closed-loop system is a safe and much more effective way for people living with type 2 diabetes to manage their glucose levels than current standard treatment with insulin. The device has been submitted for regulatory approval in the U.K. and we anticipate that this may be commercially available for people with type 2 diabetes in the next 12 months.”
Dr. Ishita Prakash Patel, an endocrinologist with Texas Diabetes and Endocrinology in Austin, not involved in this study, commented in the successful trial to MNT.
Dr. Patel called the study an “interesting topic” and noted that “the fully automated — vs. the hybrid currently available — closed-loop insulin pump is the next step we are all looking toward with excitement in the insulin pump world.”
While Dr. Patel is excited about this step, she cautioned that the study was “a small single-center study over a short time period.”
“In the future, it will be exciting to see multicenter data over longer periods of time, which will certainly come. It will also be interesting to see type 1 diabetics studied, as they typically have more insulin sensitivity, to see if hypoglycemia rates are increased in this population,” commented Dr. Patel.
“The diabetic device research field is moving steadily toward fully automated closed-loop insulin pumps,” said Dr. Patel. “This is a very exciting frontier for our insulin-dependent patients.”
“We have already seen great success with the hybrid models of pumps, but these newer models will not require [the] input of carbohydrate intake,” she noted. “Once optimized, this will make the disease more manageable and less time-consuming, while improving blood sugar control in our patients.”
Hits: 0